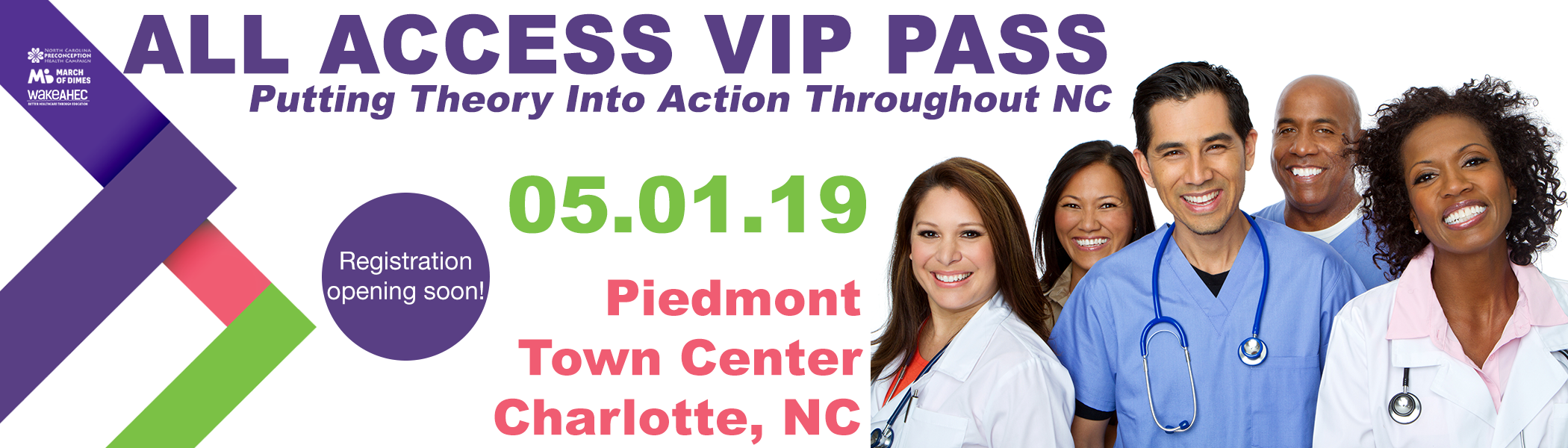
Welcome to Every Woman NC – North Carolina Preconception Health Campaign
News
Bridging Health and Accessibility
In a ground-breaking partnership that connects the realms of financial accessibility and public health, ASAP Finance...

Preconception Health Webinar Series Kicks Off Sept. 26!
The March of Dimes North Carolina Preconception Health Campaign Webinar Series is...